Melissa Walling

Like many other stories about melanoma, Melissa Walling’s journey with melanoma started with a mole on her arm. Try as she might, she couldn’t wish it away. This 27-year old was more concerned with someone else noticing her ‘ugly’ mole than with it being something serious.
“Looking back, it met all the hallmarks of melanoma,” says Melissa.
It wasn’t until her best friend noticed it that Melissa decided to do something about it.
The dermatologist removed it. Melissa was relieved; no one else could judge her ugly mole. She thought she was done with it – and moved on.
Two weeks later Melissa was confused – and frankly a bit annoyed – that the doctor wanted to see her again the next day. “Honestly, I had no idea what was coming.”
With her mother beside her, Melissa heard the news that would change her life forever: ‘You have melanoma.’
“It was a waterfall of information – I didn’t understand or wasn’t ready to hear. Either way, it didn’t click,” says Melissa. “I had cancer – but was really in denial about the entire thing.”
The severity of what she faced didn’t come into focus until a few weeks later when she learned that the lymph nodes in her right axillary (underarm) that had been sent for testing as part of her sentinel lymph node biopsy had come back positive. Not only did Melissa have melanoma, but it had started to metastasize throughout her body.
Her Mom, a nurse by training, convinced her to get a second opinion from a doctor that regularly saw and treated people with melanoma. They made an appointment and the drive to Johns Hopkins University.
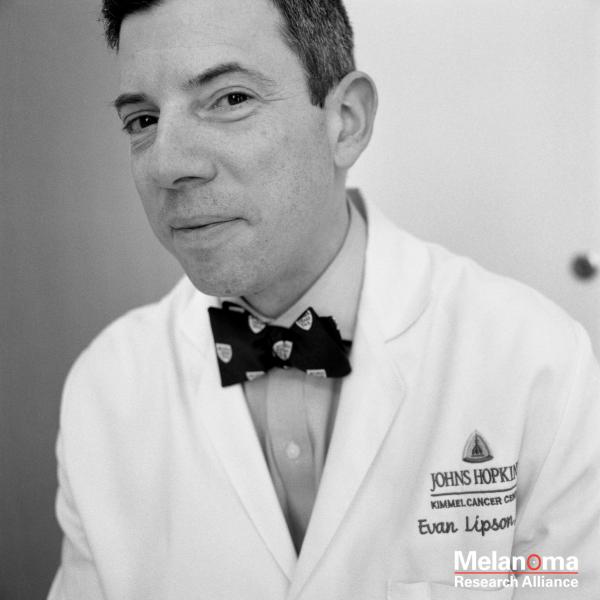
So, on New Year’s Eve, in the last appointment slot of 2013, Melissa met Dr. Evan Lipson. “It wasn’t until I met Dr. Lipson that I realized how poorly I clicked with my previous doctor,” says Melissa. “He gave me choices and talked things through with me. That’s when I started to fully understand what melanoma meant to me.”
She would need another surgery to remove all lymph nodes in her right axillary, or armpit – what’s called a Complete Lymph Node Dissection. Dr. Lipson also recommended that she follow up with a year of systemic therapy.
In 2014, Complete Lymph Node Dissection (CLND) was the standard practice in situations like this. The thinking went, by removing all of the lymph nodes that could have been affected, you could achieve better disease control and extend progression free survival. A landmark study published in 2017 in the New England Journal of Medicine challenged this conventional wisdom. In a study of over 1900 patients, researchers found no significant difference between patients who did or those who did not undergo the procedure. Today, due to the side effects associated with the procedure, like swelling in the hands and feet, CLND is only used in specific instances where additional information about the spread of melanoma is needed.
After a few weeks of recovery, it was time for Melissa to start her systemic therapy. Melissa would receive an infusion of high-dose interferon five days a week, for the first month. Then, would begin a maintenance regimen 3 days per week for another 11 months. In clinical trials, 42% more patients who received this regimen were disease free than those who did not.1 The downside, is that the therapy was difficult to manage, many patients experienced severe side effects and spent 15 – 20 hours per week in the hospital receiving the infusions.
Interferon, while not frequently used today, was the first FDA-approved adjuvant therapy for melanoma. A precursor to modern checkpoint immunotherapies, interferon is a genetically produced version of a human protein that stimulates the immune system to find and kill melanoma cells with the goal of stopping, or delaying, the return of melanoma.
“Interferon was the worst roller coaster ever,” says Melissa. “For that year, it was my life.”
And life, wasn’t easy. Melissa experienced extreme fatigue, hair loss, and nausea. Near the end of her year she even ended up in the emergency department with a pleural effusion which made it extremely difficult to breathe. “Today, I still have lymphedema (swelling) from the lymph node dissection and still have some issues with my memory and fine motor skills from the interferon,” says Melissa.
She celebrated the end of her year of interferon with a dinner that combined sushi and champagne.
Earlier this year, Melissa celebrated another milestone. After a full-body CT scan and a brain MRI, she was considered NED – or No Evidence of Disease – for 5 years.
Today, melanoma is still on Melissa’s mind. She still is closely monitored and gets a full-body skin exam every three months. She’s also needed several additional surgeries to remove other, early-stage melanomas. “In so many ways, melanoma is a never-ending battle,” says Melissa.
She also frequently volunteers with Moving for Melanoma of Delaware, a non-profit that raises awareness of and funding for melanoma.
“I go to awareness events to promote sun safety, help organize an annual 5k that raises about $100,000 each year for research, and share my own experience as a young cancer survivor with others,” says Melissa. “I feel so fortunate that I’ve been able to help other people not make the same mistakes that I did.”