David Henry

Today, life is almost back to normal for David Henry. It’s been over five years from when David was first diagnosed with Stage 3B – and then Stage 4 acral melanoma. But today, David’s melanoma is stable and his targeted therapy treatment of dabrafenib + trametinib for the past two years, continues to work.
“I think about it as a chronic condition that needs to be watched and managed,” says David. “I know that things could always change – I’m very aware of that – but right now, life is good.”
David’s outlook was not always so promising. In fact, his journey with melanoma has had some tumultuous ups and downs – which included learning to walk after a month-long paralysis episode that was difficult to manage and diagnose.
While David isn’t one to put much stock in luck, he can’t deny the almost serendipitous way that things have just worked out.
The first time that the stars aligned in his favor was when he was referred to a dermatologist for a completely harmless sebaceous cyst. At the end of his appointment, he figured ‘why not,’ and asked the doctor to take a quick look at a stubborn mark on the bottom of his foot. David explained that while the mark had been there for a long time, he’d noticed that its appearance had been changing.
“It was clear that he didn’t like what he was seeing or what I was telling him,” says David.
The doctor took a biopsy and said he’d get back in touch in a few days.
Five days later, David got a call: “Are you at home – do you have a few minutes to talk?” he remembers thinking that this didn’t sound good.
His doctor explained that the biopsy indicated that the lesion was actually melanoma and that he’d been referred to a team of specialists at Memorial Sloan Kettering Cancer Center for the next steps.
Due the melanoma’s location on the bottom of his foot, the surgery and its recovery were hard. Melanoma surgery requires wide margins and David needed a skin graft to close the wound. This was further complicated by the relatively low blood flow and position of the graft. Doctors just weren’t sure if it would take.
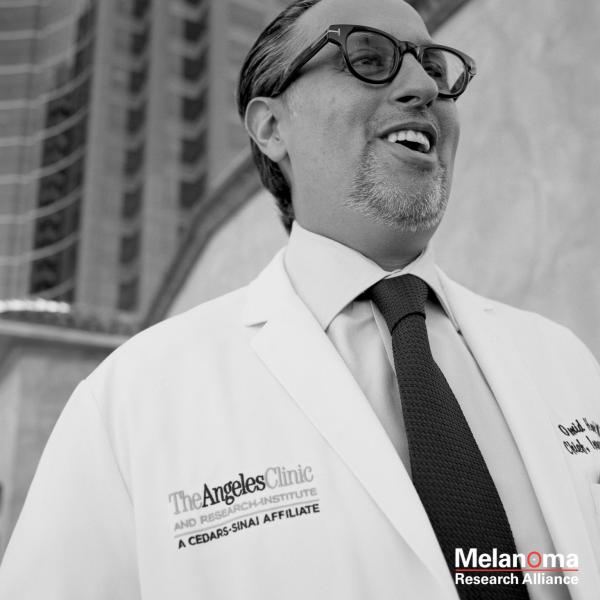
Despite this, the surgery was successful. In addition to surgery, David also needed systemic therapy to treat melanoma that had spread from the primary site, so his surgical oncologist Dr. Daniel Coit referred him to Dr. Paul Chapman. Dr. Chapman, a medical oncologist by training, is a member of MRA’s Grant Review Committee and Medical Advisory Panel. He has also been awarded two MRA grant awards.
First, they tried the immunotherapy pembrolizumab – but it didn’t work. Then, Dr. Chapman suggested a new targeted therapy combination of Vemurafenib (Zelboraf®) + Cobimetinib (Cotellic™). While both treatment approaches are effective for some patients, neither worked for David. The Vemurafenib + Cobimetinib actually landed David in Memorial Sloan Kettering’s main hospital for several days with a painful, head-to-toe rash. After stabilizing his condition, David was discontinued on the combination therapy.
That’s when insurance issues complicated everything. While at first the MSK team did everything they could to appeal, override, and work through his insurance company’s system – Dr. Chapman recognized that it wasn’t good for David or sustainable for his team. So he helped David transfer his care to Columbia University and Dr. Richard Carvajal – both part of his insurance’s network.
“I was very happy with Dr. Chapman and the care I was getting at MSK – so I was initially somewhat nervous about making this change,” says David. “Fortunately, upon my very first meeting with Dr. Carvajal – my fears were allayed. I’ve received nothing but the best while at Columbia.”
Dr. Carvajal, also a two-time MRA-funded investigator, suggested a second BRAF/MEK targeted therapy combination called Dabrafenib (Tafinlar®) + Trametinib (Mekinist®). While both treatments work similarly, they each have a distinct side effect profile. So while David responded poorly to the first– it was possible that he may not react the same way to the second combination.
After starting the new combination, David started to have balance issues. The breaking point was when he found himself stuck in the New York Subway unable to navigate the stairs. By the time he got to the Emergency Department at Columbia’s Milstein Hospital, his balance was progressively worsening.
Soon, David lost feeling in his feet altogether, and the paralysis began advancing further up his body. His doctors had never seen a reaction like this, but they weren’t taking chances. A respirator was standing by just in case he lost the ability to breathe on his own. Fortunately, through a combination of steroids and other medications, David’s doctors were able to stop the paralysis progression. Unfortunately, they couldn’t reverse the paralysis. He would just need to wait and hope that it would subside.
David was paralyzed – from the waist down – for nearly a month.
Experts believed that this episode was actually an extreme example of what they call an immune-related adverse event, likely caused by the immunotherapy agent pembrolizumab that David had had months earlier. Put bluntly, his immune system – spurred by the immunotherapy – had attacked his central nervous system.
Once he regained feeling, David needed months of both physical and occupational therapy. He needed to learn how to walk again.
Now, back in Dr. Carvajal’s office, David was being asked to try the dabrafenib + trametinib combination one more time
“He made it clear that they didn’t think what happened last time would happen again,” says David. “Ultimately, I told him – I’m in your hands. If that’s your recommendation – I’m happy to go along with it.”
This was another serendipitous moment in David’s melanoma journey. This time, his body tolerated the targeted therapy combo. The side effects he did have, fever and fatigue, were manageable with medication – and two years later – his melanoma is stable.
“I’ve been told that about 20% of patients on targeted therapies are able to ‘beat the odds,’ and do better than expected for longer than expected,” says David. “All signs point to me being part of this group.”
Of the five years that melanoma has been part of David’s life, 2019 has been the best yet. He started cycling again – something that he was very avid about prior to melanoma entering his life. David even joined the ‘Phase Oneders,’ a team of doctors, researchers, nurses, and patients led by Dr. Carvajal for a charity biking event to raise money for research at Columbia.
“I’m not going to be racing up a mountain any time soon,” says David. “But I’m glad that I’ve been able to rediscover how much I enjoy cycling.”
David has also fallen in love with change-ringing, a specific method of ringing tower bells that merges math, music, and coordinated- group exercise into a music that originated in 17th century English churches. “Working as a team to create something that has existed for hundreds of years – it’s powerful,” says David.
“I know that I’m in the best hands for care and treatment – and that really gives me cautious optimism about my future. I know that things can change in an instant – but am so grateful for the research that has allowed me to get to this point. I wouldn’t be alive today without it.”
Without you, melanoma research can't happen. Learn more about clinical trials.
Please support MRA's mission to end death and suffering due to melanoma. 100% of your donation will go directly to funding innovative melanoma research, without any overhead, admin, or fundraising expenses.